The seven skilled nursing facilities in United Hospital Fund’s polypharmacy learning collaborative recently came together to discuss successes, ongoing challenges, and learn more about an approach that puts residents at the center of care. Now in its second year, the learning collaborative explores how to reduce the burden of overprescribing in nursing homes.
Polypharmacy is the prescribing of an inappropriately high number of medications that may increase adverse outcomes like drug-drug interactions, falls, cognitive impairment, and hospitalization. The participating facilities are designing and implementing strategies to better monitor and assess medication regimens and prescribing practices. They are also looking at the use of deprescribing—the practice of withdrawing patients from certain medications, supervised by a health care professional, with the goal of improving outcomes.
The project is funded by the Mother Cabrini Health Foundation, with additional support from the TD Charitable Foundation. Its first learning session of 2023 was held in March, its second in June, and the third and most recent on September 19 at UHF’s office.
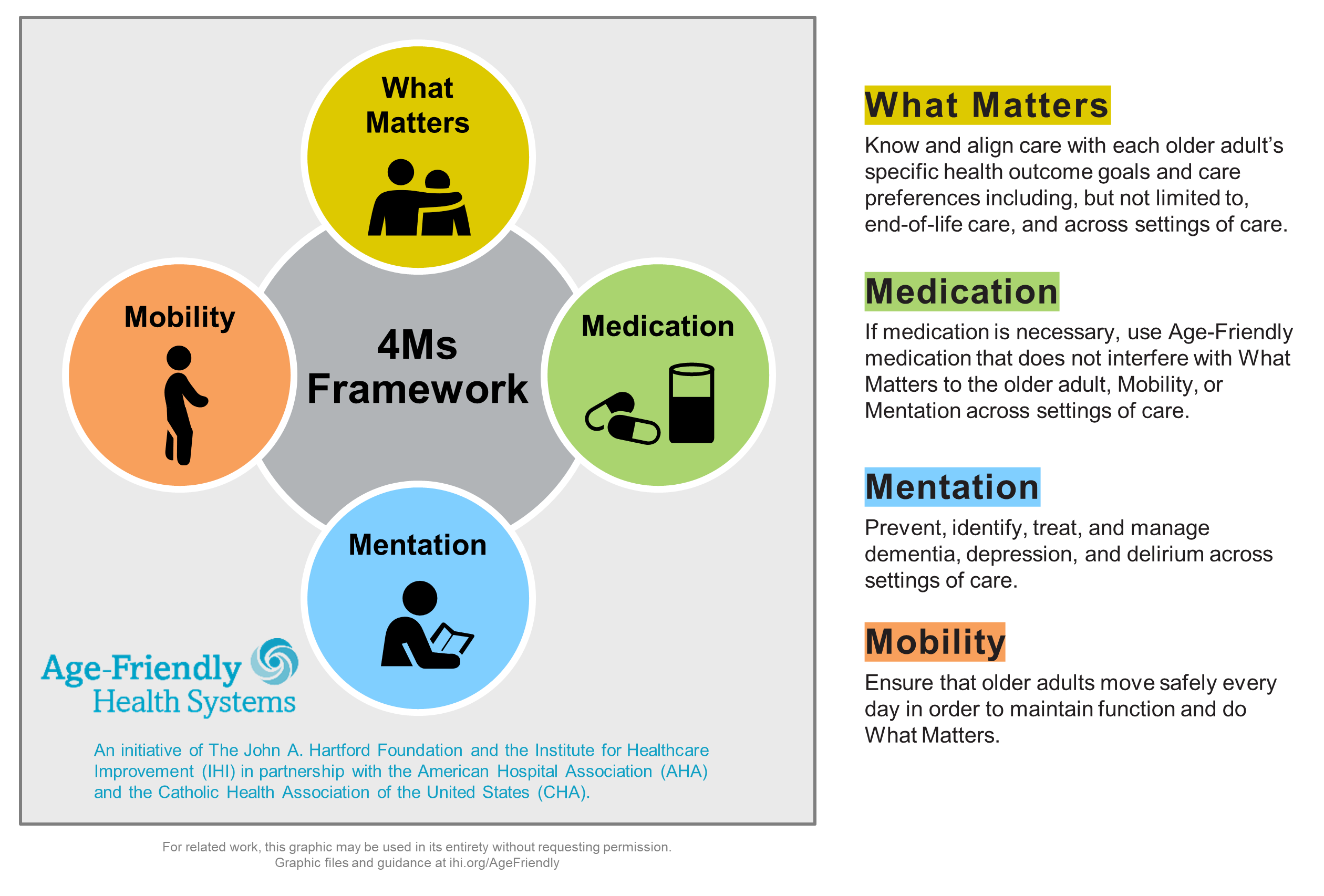
The first portion of the meeting featured a presentation by Alice Bonner of the Institute for Healthcare Improvement (IHI) on the challenges and opportunities for nursing homes in using a framework of patient-centered care known as Age-Friendly Health Systems. The model provides a set of four evidence-based principles aimed at improving care for older adults, known as the four Ms: What Matters, Medication, Mentation, and Mobility. Dr. Bonner, PhD, RN, FAAN, FAANP, focused on how consideration of all the 4Ms is important in medication management.
She noted that “age-friendly is a continuous process—it’s not one and done.” She shared several success stories of using the approach as well as challenges, including staffing issues and communications hurdles. “It makes a difference if it’s part of policy and culture,” said Dr. Bonner, who is the senior advisor for aging at IHI.
Several participants shared their experiences using the 4 Ms and stressed the importance of building trust with patients and families and caring for the patient as a whole person, rather than treating symptoms. One participant said his facility was posing “What Matters” questions with pictures of “What Matters” posted at the foot of each patient’s bed.
Learning collaborative faculty member Jenn Pruskowski, PharmD, MS, BCPS, BCGP, CPE, also led a discussion on how “What Matters” questions can help providers identify deprescribing opportunities by better understanding patients’ life contexts, priorities, and treatment goals. Some questions might include: “What brings you joy? What makes you happy? What makes life worth living?”
The collaborative’s other faculty member, T.S. Dharmarajan, MD, told the attendees that “deprescribing is going to be the wave of the future” and added that “the facilities who have participated will be ahead of the rest.” Dr. Dharmarajan is vice chairman, department of medicine, clinical director, division of geriatrics, and the program director, geriatric medicine fellowship program at Montefiore Medical Center; he’s also a professor of medicine at the Albert Einstein College of Medicine.
UHF recently published its 2022 findings in a report, Reducing the Risk: Year 1 Report of the Polypharmacy in Nursing Homes Learning Collaborative, which also included tools and recommendations for other organizations wishing to develop their own deprescribing initiatives.